Do you routinely scan the abdominal aorta as part of your standard transthoracic protocol? Is this common practice?
Here is a case that may encourage you to include it in your scan
Disclaimer: Although the images are real, dates, places and people have been changed to protect the patient confidentiality.
Patient: Male late 60’s, presents with dyspnoea on exertion for three months. Referred for echo. No cardiac or vascular history. Normotensive. Normal BMI/BSA, no history of smoking or excessive alcohol intake. Normally fit and healthy. Normal blood results including BNP.
Full transthoracic echo performed. Main findings are normal LV and RV systolic function, normal valve function. bi-atrial dilatation. Grade II LV diastolic dysfunction and a moderate probability for PAH. So far, nothing too unusual. Likely cause of symptoms found.
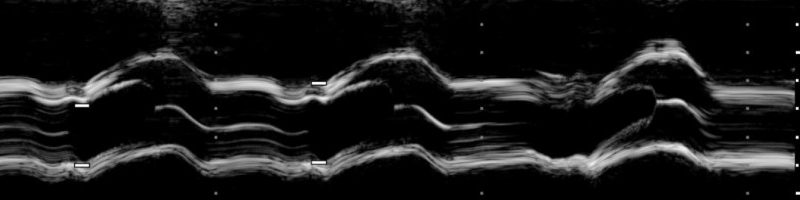
The last part of my standard scan is to visualise the mid abdominal aorta. Easily achieved with the echo probe, a quick inferior tilt of the probe and there it is. However this time, the aorta is abnormal

A little colour Doppler confirmed I was looking at the abdominal aorta.
I turned to the patient and asked if he had ever had and abdominal scan or screening for the aorta. He denies either, as does his wife. So what is an echocardiographer to do?
The current NICE guidelines for AAA repair are >55mm (asymptomatic). This aneurysm is large at 6.4cm and there is a rather large thrombus noted, although the patient is asymptomatic. This finding warrants an urgent referral, within two weeks, to the vascular department for a full abdominal scan and possibly a CT and then on for urgent surgery.
The use of anti-thrombotic therapy is determined by a number of different criteria and requires a careful and considered approach that assesses aortic wall and thrombus stability

According to NICE, screening studies in the UK show an estimated prevalence of 1.3–12.7% depending on the age group studied and the definition of AAA. But because they are often asymptomatic, the prevalence may well be higher than that suggested by NICE. So the take home message is, always look at the abdominal aorta at the end of an echo. Your probe is already positioned at the subcostal window. It takes two seconds, but you could end up saving someone’s life.

Leave a comment