SOME HELPFUL HINTS AND REFERENCES
Basics
- Always record the patient’s height, weight and blood pressure
- Comment on technical quality
- List the clinical indications
Use of language:
Language is important in echocardiography. The terminology we use is specific and descriptive but must also be professional and concise. The use of standard terminology across the echo world ensures that an echo performed in one county reads the same as an echo in another. It brings consistency and accuracy to the profession.
There are certain phrases and descriptors that are standard in echo reporting – see the examples below.
- Good leaflet excursion
- Structurally normal
- Mild/Moderate/Severe
Other terms are less standard but should be utilised when we are not dealing in absolutes.
We use terms such as Appears or Likely as descriptors as you cannot always be definite in your assessment.
An example of this is the reporting of the right heart valves as every facet is not seen on echo. The PV is only ever seen in cross-section and the TV is rarely seen en-face. To report these valves then we use the term “appears normal” as we cannot be 100% sure.
When reporting the echo, remember who your audience is. The main body of the report should be written in compliance with the full technical specification guide and is aimed at a fellow echocardiographer/cardiology specialist. It should include comments on all cardiac structures and valves, avoiding visual assessments where possible, and only include values which do not appear in the measurements page to avoid repetition.
LV:
- Comment on chamber size using a biplane volume indexed to BSA if possible, but also comment on chamber geometry. The LV should be conical shaped, if it is abnormal in shape, then this is an indication of pathology.
- Comment on wall thickness and appearance – distribution of hypertrophy, presence of trabeculations etc
- Comment on any regional wall motion abnormalities – if not all areas are seen, state – unable to completely exclude regional wall motion abnormalities from these images, but state areas that are seen if they are abnormal
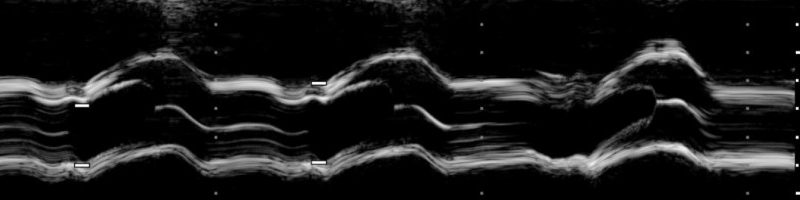
- When assessing global systolic function you should take in to consideration both the radial and longitudinal function, as well as haemodynamics and the effect of valve disease on function. Please refer to BSE guidelines for accurate assessment
- Where possible measure the LVEF by Simpson’s biplane or 3D volume analysis, if this is not possible give a visual assessment (5 % range) and quote the reason for not being able to measure the EF
- Diastolic function assessment is currently under revision by the BSE, until we have further guidance, we currently assess diastology by grade using mitral inflow, left atrial size, pulmonary vein flow and TDI assessment. We grade it as normal, grade I, II or III. There are some departments that like the use of qualifiers such as mild, moderate, and severe. It is recommended to use the grading system, but the addition of these qualifiers may assist the clinician reading the report in their interpretation.
- If there is pathology present, then please comment on diastolic function in the context of that pathology
ATRIA
- LA: The recent change to the normal values now classifies the LA as normal, borderline dilated and dilated. Where possible this should measured by a biplane volume and indexed to BSA. A diameter should be measured also as this parameter is still relevant in some clinical scenarios (ie EP)
- RA: Measured in the focused right heart window as an area indexed to BSA, the RA is reported as normal or dilated.
- Comment if there are any normal variants seen such as Chairi network, Eustachian valve and comment that this is a normal variant
- Comment on atrial septum: Comment on appearance – ie lipomatous thickening/mobile/aneurysmal IAS.
If shunt is present please calculate Qp:Qs but only in the absence of any valve regurgitation. Describe the shunt jet – direction, volume and extension into the cavity. Comment on flow velocity across the defect.
RV:
- When reporting the RV, attention should be paid to both longitudinal and radial function and measured appropriately in the RV focused window. The report should comment on cavity size and wall thickness, regional wall motion, longitudinal function, radial function and then an overall assessment of global function
- Include assessment of the RVOT diameters when assessing RV size, also include this region when assessing for RWMA
- Comment if there is any pacemaker artefacts seen, such as leads.
- Comment on IVC here – size / respiratory response and the associated RAp
- Quote PASP here as a range and comment on probability for pulmonary hypertension as per the BSE guidelines. Add in measurements such as MPI or PVR as appropriate
Valves:
- AV: number of cusps, structure of cusps, cusp mobility, forward flow/velocity – degree of stenosis and Doppler values/valve area, appearance of regurgitation – volume/flow convergence/direction of jet etc
- MV: Structure of leaflets, leaflet mobility, forward flow, appearance/direction of regurgitation – pulmonary vein flows, PISA and EROA if indicated. Stenosis – Calcific or Rheumatic, mean gradient and valve area by PHT
- TV: Structure of leaflets (best to say ‘Appears normal’ if not seen in SAX), leaflet mobility, forward flow, appearance of regurgitation – hepatic vein flows, PISA and EROA if indicated, stenosis is very rare but can happen so use the BSE values to assess severity
- PV: Comment if not clearly visualised as is common: comment on Doppler, presence of regurgitation and forward flow/velocities. Include assessment of acceleration time as either normal or reduced. Comment on mPA diameter. Both of these measurements are part of the PAH probability assessment
Notes on valve reporting:
- For regurgitation – where possible comment on the quantity and the mechanism of the regurgitation (if you cannot see the mechanism such as prolapse, thickening, annular dilatation etc, state mechanism unclear – this is for mild/mod/severe regurgitation – where possible, back up with measurements
- Quantify any stenosis according to guidelines and where possible back this up with gradient and valve areas. For AS, the Pedoff (stand alone) probe should be used when possible for all gradients of moderate or more. Aortic valve gradients should be obtained from at least 2 different windows (apical, arch or RSB) – quote on your report where the peak gradient was obtained.
Other findings:
- In this section you should add any additional information to complete your report
- Comment on aorta: Please comment on all levels of the aorta if seen – Root measurements should be indexed to height, all other measurements are absolutes unless the patient is possible Marfan’s then please use the BSE protocol on Marfan’s patients. On the protocol it lists the other dimensions and their normal height indexed values – this only applies to this cohort of patients
- Comment on pericardium: comment on appearance, thickened/echo bright etc. Any effusion – comment on location, size and haemodynamic compromise. Evidence of epicardial adipose – comment on location and size
Conclusion:
The conclusion should be a clear and concise summary of the main report findings. This section should condense the important and relevant information in an easy to read and understandable paragraph, which should not have any abbreviations. The summary should answer the referral question and tell the story of the scan,
At a minimum: Comment on the LV function (systolic and diastolic, where appropriate). Comment on the valves and the right heart.
Conclusion examples:
Patient referred with SOB and murmur
- Sinus rhythm at 70bpm
- Normal left ventriclar size, normal wall thickness and normal systolic function. Likely normal diastolic function. Normal left atrial size
- All valves appear to function normally with only trivial physiologically normal mitral and tricuspid regurgitation noted.
- Normal right ventricular size and function, normal size right atrium, low probability for pulmonary hypertension
Patient referred with murmur and LVH on ECG.
- Sinus Rhythm at 65bpm
- Moderate aortic stenosis
- Normal left ventricular size, mild concentric hypertrophy, and globally good systolic function. Grade I diastolic impairment and left atrial dilatation.
- All other valves appear structurally and functionally normal.
- Normal right ventricular size and function, normal size right atrium, low probability for pulmonary hypertension
Pt referred with SOBAR and raised ProBNP
- Sinus Tachycardia at 110bpm
- Severely dilated left ventricle with evidence of adverse remodelling and severely impaired global systolic function. Elevated filling pressures. Severe functional mitral regurgitation and a dilated left atrium.
- Mildly dilated RV cavity size with moderately impaired systolic function, moderate functional tricuspid regurgitation, right atrial dilatation and a high probability for pulmonary hypertension.
- Aortic and pulmonary valves appear to function normally.
As you can see, the conclusion marries together the findings into a fundamental finding or diagnosis. Please learn to write conclusions in this manner rather than copy/paste the comments from the main body of the report.
Resources
Published by Katherine

Leave a comment